You have probably heard it said the nutrition and health status of dairy animals are unmistakably linked to one another.
In the same way we humans lose our appetites when sick, or feel poorly when our diets are unhealthy, proper nutrition is required for a cow’s immune system to function adequately. Likewise, a cow’s immune status influences the direction of nutrients in the body.
Gut health specifically is correlated to optimal performance in dairy animals, with up to 70 percent of a cow’s immune response protecting the gastrointestinal tract.
From the time of a calf’s birth, bacteria begin to colonize its intestines. Not all of these bacteria are “bad”; in fact, most are beneficial. The volatile fatty acids produced by bacterial fermentation serve to lower the pH of the intestines and inhibit growth of potential pathogens.
Some of the beneficial bacteria act as a barrier alongside intestinal mucosa tissue, and other bacteria even produce antimicrobial compounds to protect the cow. Balance among intestinal microflora is crucial to optimal health and production. Many environmental or management factors may disrupt the balance of intestinal bacteria in a dairy cow, such as:
- Pathogens
- Stress
- Metabolic upset
- Antibiotic use
- Commingling
Two harmful bacterial pathogens, salmonella and clostridia, cause significant gastrointestinal problems in dairy animals, ultimately leading to economic losses or death loss on farms.
Salmonella
Most people are familiar with salmonella, since it is one of the most serious foodborne bacteria for humans in the U.S. Dairy cows are no exception and, oftentimes, the on-farm presence of this damaging bacterium goes unnoticed. In a multi-state study across conventional and organic dairies, almost 90 percent of operations had at least one positive cow, and 5 percent of cultured cows were positive.
Cows may not show any symptoms of salmonella infection when shedding the bacterium through their manure, even shedding to the same degree of cows that do appear sick. Following recovery, cows may shed the organism for many months, despite showing no outward signs.
Furthermore, flies, dogs, rodents and birds may also be sources of infection. Even contaminated vehicles, gates and equipment can be sources of spreading the bacteria around the farm.
During acute infection with salmonellosis, an animal will exhibit high fever, serious diarrhea which often contains blood and severe dehydration, which can lead to death. Prevention of this disease is incredibly important because treatment with antibiotics alone is typically not sufficient to overcome the effects of dehydration.
Clostridium
Clostridial bacteria differ from salmonella in that they are naturally present in the gut flora of healthy cows. In other words, the mere presence of the bacteria does not pose a problem, and animal-to-animal contact does not spread clostridial diseases. Clostridia only become harmful when certain stressors/events are present which provide the opportunity for over-growth.
Circumstances conducive to the growth of these bacteria, and subsequent release of toxins, include heat stress, dietary stress, injury, management changes and poor parasite control. Several diseases are attributed to different species of clostridial bacteria:
- Lockjaw
- Gas gangrene
- Malignant edema
- Jejunal hemorrhage syndrome (Bloody gut)
- Sudden death
- Abomasal ulcers
- Blackleg
- Red water disease
For most of these illnesses, treatment success is rare due to their aggressive nature, which makes prevention key. Many operations vaccinate against clostridial diseases; however, without a booster vaccination within six weeks, this is inadequate protection.
For young calves, protection should be aimed at providing colostrum from vaccinated dams rather than vaccination of the calves themselves.
Management prevention strategies
Often, the first response of producers to bacterial infections is antibiotic treatment. However, consumer concern about use of antibiotics on farms has limited this treatment option now and into the future. In addition, some species of salmonella are resistant to multiple antibiotics, and clostridia bacteria will often kill an animal before intervention can take place.
The most prudent method for protecting dairy operations against clostridium and salmonella is proper health management before disease hits. The management strategies for prevention of gastrointestinal insult from these pathogens include, but are not limited to:
- Separating sick, treated or cull cows from fresh cows
- Including ionophores in weaned-calf or bred-heifer diets
- Rodent control
- Consistent feeding practices
- Vaccination where applicable
- Appropriate storage and fermentation of silage
- Short-term use of calving area by calving cows only
- Sanitary conditions for colostrum feeding
- Limited antibiotic use
- Maintenance of healthy gut flora by inclusion of an active microbial in the diet
Active microbials
Referring back to the importance of gut health and balance of the gut microbial population, feeding additives that contain microbial species is one nutrition management strategy consistent with the industry’s transition toward less antibiotic use.
Active microbials, direct-fed microbials and probiotics are interchangeably used terms which describe “a live microbial feed supplement which beneficially affects the host by improving its intestinal microbial balance.”
Benefits of active microbials in humans and animals alike are widely reported in scientific literature. Some of these include:
- Altered intestinal bacterial populations
- Improved resistance to disease
- Reduced shedding of pathogens when challenged orally
- Increased intestinal immunity
- Reduced disease symptoms
- Improved health
Choosing a strain
When choosing an active microbial, it is important to consider the strain and its activity in the intestinal environment based on research. Some products may contain multiple strains of organisms, making it difficult to ascertain which strain is responsible for the positive effects.
Research conducted on individual strains can help you choose a product that will target the desired benefits for your operation. A few examples of active microbial strains supplemented to ruminants are Lactobacillus acidophilus, L. lactis, L. plantarum, Enterococcus faecium and Bacillus subtilis. Additional selection criteria could include:
- Clear understanding of the mode of action
- pH sensitivity
- Pathogen inhibition
- Compatibility with antibiotics, coccidiostats and organic acids commonly used in the animal feed industry
- Thermostability
Bacillus subtilis PB6 for aiding in the prevention of salmonellosis and clostridial diseases
Bacillus subtilis PB6 is a unique, naturally occurring, spore-forming micro-organism. This active microbial helps maintain the balance of microflora in the intestinal tract of livestock. The above image demonstrates the inhibition of Clostridium perfringens by PB6.
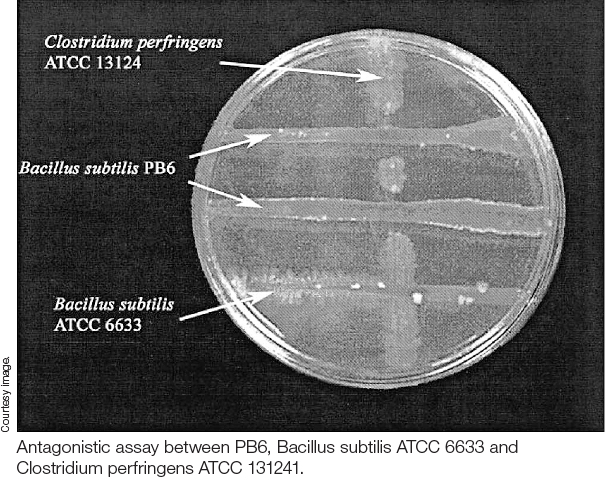
In vitro research conducted on Bacillus subtilis PB6 has shown antagonistic activity toward clostridial isolates from poultry, swine and equine sources. Recently, weaned Holstein steer calves were supplemented with PB6 in a starter ration for 35 days prior to a Salmonella typhimurium challenge.
Calves that received the active microbial displayed lower rectal temperatures and significantly reduced salmonella concentrations in portions of the intestinal tract 96 hours post-challenge compared to calves that did not receive the PB6.
Conclusions and practical application
Maintaining gut health in your dairy herd is vital to optimal performance. Adding active microbials to your ration can help balance the intestinal flora of your animals and may aid in limiting potentially harmful pathogens like clostridia and salmonella.
As the industry moves toward less antibiotic use, consider feeding safe alternatives such as live microbial feed supplements to support cow health and performance. ![]()
PHOTO 1: Bacillus subtilis PB6 in the intestine.
PHOTO 2: Antagonistic assay between PB6, Bacillus subtilis ATCC 6633 and Clostridium perfringens ATCC 131241. Courtesy images.
References omitted but are available upon request. Click here to email an editor.

-
Drew Dickson
- Product Manager
- Kemin
- Email Drew Dickson








