The good news: Dr. Heather White, an associate professor at the University of Wisconsin – Madison, might have some solutions thanks to new research on ketosis prevention and treatment.
White originally shared this information in her presentation, “Integrated subclinical ketosis detection tools: New tools to guide intervention,” at the Form-A-Feed annual conference Jan. 17-18, 2019 in Red Wing, Minnesota.
Detecting and treating subclinical ketosis
First off, producers need to decide how they plan to track ketosis in their herd. There are a number of options available, with blood tests being the most accurate. Blood tests, however, are time-consuming and not necessarily the best tool for whole-herd monitoring. The other testing options (see Table 1) vary greatly in terms of price, sensitivity and specificity.
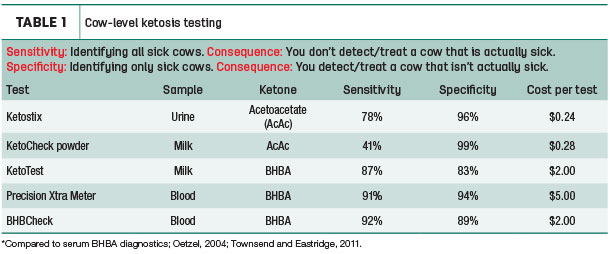
Aside from cost considerations, the big question producers need to ask is whether they prioritize sensitivity or specificity. The more sensitive a test is, the better it is at identifying sick cows, but it will likely catch animals that may not need to be treated. Specificity means the test will only be positive for sick cows; however, since it isn’t as sensitive, farms may miss some of the more mild cases. Since ketosis treatments are relatively inexpensive, White said treating a few extra cows isn’t necessarily a major concern with ketosis.
One other consideration is the scale used on the test. White said she prefers tests that use a number, as they are less subjective than a color test. This is especially important when multiple people are testing the animals, as people might disagree about a color being pink versus purple, but a number 2 will always be a 2.
Herd-level monitoring
Subclinical ketosis predictions are useful on a herd level, but they are not effective at identifying individual cows. The predictions are based on milk analysis and data exported from farm management software. Predictions can be incorporated into monthly DHI testing and are useful to:
- Allow you to monitor prevalence relative to an alarm level (above 10 percent) or goal
- Identify changes in prevalence that could otherwise be missed
- Know when to start or stop individual cow diagnostics
- Observe the benefit of a change
- Help identify risk patterns on your farm (Example: long dry period)
The challenge, however, is: This only tests cows on a herd level and doesn’t tell farms which animals to treat. As long as the farm is below the 10 percent threshold, this is fine, but once the farm hits alarm level, they need to also include individual testing (see Figure 1).
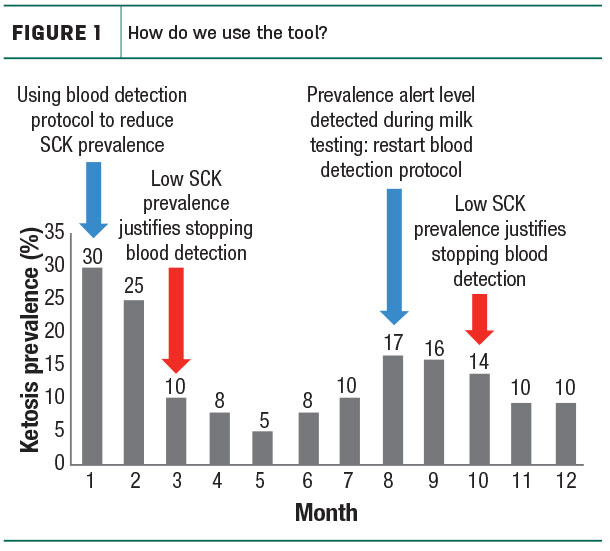
The problem is: Many farms still only do this once a month, but if a cow is going to test positive for subclinical ketosis, she will do so within the first month after calving. This means that, at best, a farm will only catch 50 percent of cows with subclinical ketosis. Instead, White proposed producers test cows weekly for the first four weeks postpartum and lower it to monthly testing after. This enables them to catch cows when they are most vulnerable without too much added expense.
When it comes to testing, White said with diagnostic testing, the goal is for the test to be 90 percent sensitive and 90 percent specific. Currently, blood tests remain the gold standard for this, but taking blood samples can be time-consuming, costly and more difficult to incorporate into a farm’s regular routine.
This is where milk testing might be a great option for some dairies. Milk samples have only 81 percent specificity and 83 percent sensitivity, but they don’t require additional cow handling, making them easier to integrate into the dairy’s day-to-day operation.
Individual cow treatment
For cows and heifers that test between a 1.2 and 3.0 millimolar (mM), she suggested a 300-milliliter oral propylene glycol bolus once a day for three to four days, but no more. A week later, check the cow again to see if she needs a second round of treatment.
For cows that test at 3.0 mM or greater, give them an oral propylene glycol bolus as well as 250 milliliters intravenous of dextrose. B vitamins and a fresh cow drench can also be added. White advised against giving the cow more than 250 milliliters of dextrose, as it could trigger the cow’s liver to reduce glucose production, causing the cow to crash again 24 hours later.
Keep in mind, the dextrose must be administered through an IV and propylene glycol through an oral drench. While it might sound like a good idea, White said that when either one is mixed into feed, it is not processed the same way and will be ineffective at helping the cow come out of ketosis.
New nutritional strategies to reduce ketosis on a herd level
In the last few years, White has conducted or been involved with a few studies at the University of Wisconsin and the University of Florida looking at nutritional options that could prevent or alleviate ketosis. The two they’ve focused on are ammoniated lactate and rumen-protected choline. Both of these options are mixed into the cows’ feed. While they may not completely eliminate ketosis, they should hopefully reduce its prevalence within the herd.
It is known that lactate helps the cow produce glucose. Historically, however, determining how to feed it has been a challenge. White said other studies have looked at feeding lactic acid to cows, but this caused their rumen pH to drop, creating a whole new set of issues. A newer option they’ve started researching, ammoniated lactate, works by providing the cow with glucose precursors, making it easier for her to produce glucose and improving feed efficiency on farms with a high prevalence of ketosis.
Their study showed a drop from 60 percent incidence rate in the herd to only 37 percent without a loss in body condition score. The cows also maintained milk production and didn’t show a drop in dry matter intake. They also had increased glucose concentration and milk lactose outputs. Overall this resulted in improved feed efficiency. White said that while this is currently a viable option for farms with ketosis challenges, she’d like to do more testing on it to explore what happens if the glucose precursors are available when the herd does not have a 60 percent ketosis incidence baseline.
Rumen-protected choline is another viable option, White said. In their study, cows received rumen-protected choline 21 days pre-calving through 21 days post-calving. The result, cows averaged an extra 5 pounds of milk per day for their entire lactation. The choline also helped decrease liver fat, improving liver cell function, which they believe led to the higher milk production.
To top it all off, the supplement positively impacted the dam’s calf. In fact, calves born to these dams had better growth and were healthier than calves born to dams that had not received the rumen-protected choline supplement. White said she hopes to repeat this study soon to further explore the full implications of rumen-protected choline supplementation on the cow and calf.
While ketosis might never be fully eliminated from the herd, through regular testing and a treatment program that focuses on giving the cow the tools to help herself, ketosis can be greatly reduced in today’s dairy herds. ![]()

-
Jenna Hurty-Person
- Field Editor
- Progressive Dairyman
- Email Jenna Hurty-Person






