As a dairy veterinarian, I agreed with her statement and felt it deserved further investigation. I became aware of an ongoing field study by veterinarians Scott Crain and Robert Coffey on OS in feedlot cattle. They were seeing higher incidences of certain diseases and joint issues in late-day-fed feeder cattle. I suspected something similar was happening to dairy cattle in mid- to late lactation and, to try to prove this, I conducted a similar study in dairy herds.
What is oxidative stress and why is it so harmful?
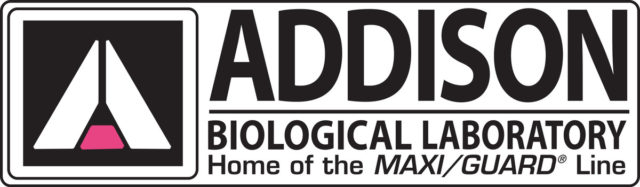
All cells must produce energy in order to survive. The process cells use to produce energy is called cellular aerobic metabolism. However, in addition to producing this energy, some toxic byproducts called reactive oxygen species (ROS) or free radicals are created. These ROS can bind DNA, proteins and cell membranes, causing cellular damage and death. Oxidative stress occurs when the levels of ROS exceed the ability of the body’s own natural antioxidant systems to detoxify them.
Three enzymes (catalase, superoxide dismutase and glutathione peroxidase) and their co-factors (copper, iron, zinc, manganese, selenium, magnesium and glycine) are critical in detoxifying these free radicals in the body. If the minerals and co-factors become depleted by overwhelming levels of ROS, then these neutralizing reactions will stop, and OS damage will result (see Figure 1).
OS occurs in cattle during periods of stress, high energy production and rapid growth. If left uncontrolled, these effects can add up over time, and cattle can develop a number of clinical and subclinical diseases and production issues.
What diseases are caused by OS?
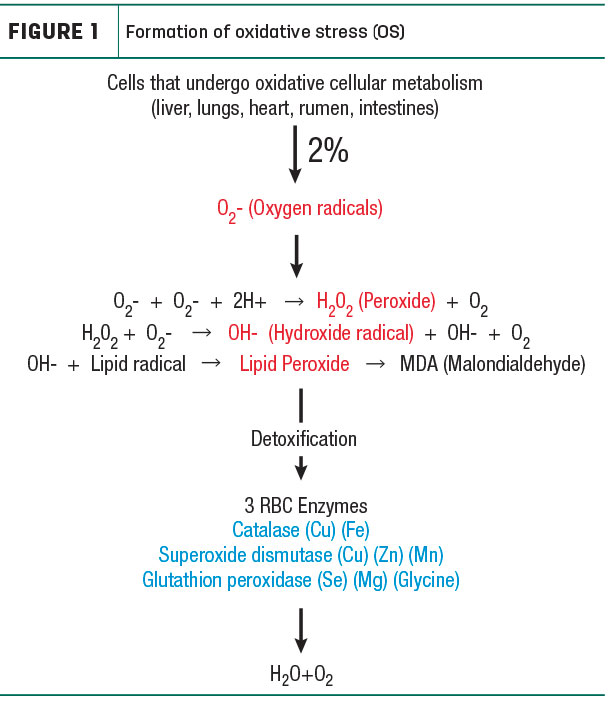
The resulting disease state will be a reflection of the organ or tissue damaged by the excess toxic ROS. For example, if the immune system is targeted, we can see metritis, retained placentas and mastitis. Damage to the lungs can result in interstitial pneumonia and Mycoplasma bovis specifically as a result of high peroxide, a type of ROS. OS can also lead to lameness due to laminitis and joint inflammation. This joint destruction constitutes a humane issue when you realize the widespread incidence.
In his 2018 field study, Dr. Crain examined the knee joints on more than 3,500 necropsies and more than 5,200 carcasses audited in feedyards and packing plants across the Midwest to evaluate the prevalence of joint lesions associated with osteochondrosis (OC) in fed cattle. Dr. Crain found that close to 90 percent had joint erosions due to OS. I went to a dead stock processing plant and randomly opened 14 knee joints and found the same type of erosions on 100 percent of those sampled (see Figure 2).
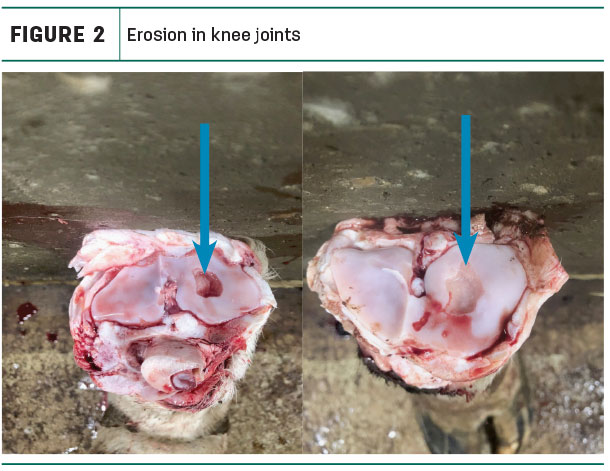
Even more significant is the role OS plays when it damages the gastrointestinal tract (GIT) and leads to the formation of “leaky gut.” The cells lining the GIT are connected by tight junctions which are disrupted by inflammation and cell damage caused by OS. As a result, bacteria and endotoxins are then absorbed systemically and can lead to many disease conditions (see Figure 3).
Common practices such as overcrowding, inadequate effective fiber, increased HMSC, as well as slug feeding and sorting can all lead to a decrease in rumen pH, which contributes to increased ROS and leaky gut.
What are the effects of OS on production?
The way OS affects production is best described by the hepatic theory (HOT) by Dr. Mike Allen of Michigan State. OS can change the way cows respond to insulin. Post-fresh cows oxidize excess non-esterified fatty acids (NEFA) and propionate (corn), causing inflammation leading to decreased appetite and insulin resistance. This can cause increased incidence of metritis, fatty liver and ketosis resulting in lower peak milk and reduced first-service conception.
In post-peak cows, OS increases insulin sensitivity at the cellular level, causing cows to divert more energy to their backs than their udders, thus reducing milk production. The bottom line is: OS decreases persistency post-peak. For example, a 2 percent decline in persistency could result in 2,600 pounds less milk.
How to prevent and treat OS
Prevention and treatment of OS can be achieved through supplementation of the minerals or co-factors that get depleted in the detoxification of ROS (see Figure 1). The mineral supplement I used was formulated as an amino acid chelate. The chelate form provides stability and protection to the mineral during its transit through the rumen. The amino acid part of it is recognized by the lengthy jejunum and ileum and gets readily absorbed, taking the mineral in with it. These absorbed minerals can then become rapidly available to replenish the cow’s natural detoxification processes. In contrast, non-chelated minerals only have the opportunity to be absorbed in the duodenum, the shortest part of the small intestine.
Proof that dairy cows have OS
Blood samples to check for malondialdehyde (MDA), a biological indicator of OS levels (see Figure 1), were drawn from 160 cows. The cows were from two large, well-managed herds with sampling from four groups of animals (pre-fresh, post-fresh, DIM 60 to 90, DIM 250 to 280) with half being heifers and half being cows. Sample results revealed MDA levels in dairy cows even exceeded levels found in the beef cattle and that levels were highest in mid- to late lactation (see Figure 4).
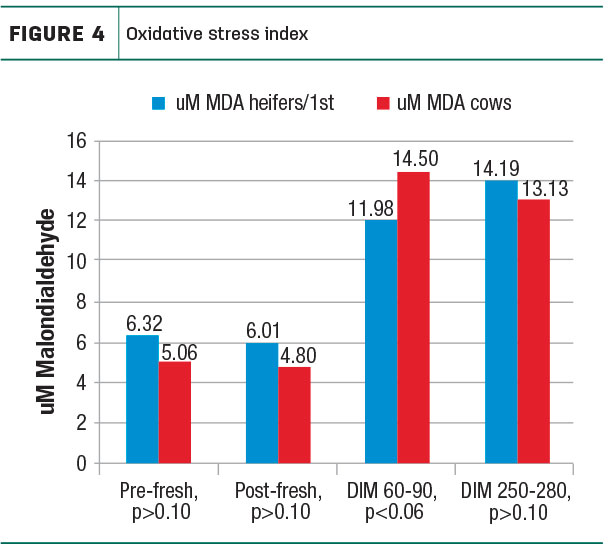
This is significant because in Dr. Crain’s beef study, diseases were seen when MDA levels reached 6 micrometer (uM), and severe disease or death was seen at 10 uM.
What is the return on investment (ROI) of supplementing amino acid chelates for OS?
After 60 days of supplementation, MDA levels were rechecked, and all four dairy groups showed a 25 to 50 percent reduction (see Figure 5).
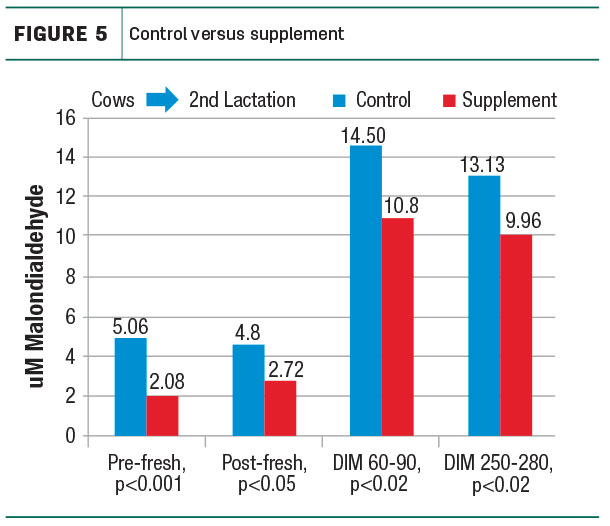
The ROI of supplementation was looked at as it related to herd health and production. First, we looked at total drug costs to see how it reflected disease incidence in the herd. Analysis from three farms where supplement was used showed up to a 38 percent reduction in total drug costs as compared to the previous year without supplementation.
A recent update from one of the herds studied showed a 50 percent reduction in veterinary/drug costs from $105,000 to $52,000 after one full year of supplementation. From a production standpoint, we saw a significant increase in post-peak persistency. In one herd where BST was withdrawn four months earlier, we saw only a 2 pound overall drop in milk production as compared to the 10 pound drop that would have been expected.
In conclusion, while OS is still a mystery to most, it leaves a huge hidden footprint in the dairy industry. Further study and understanding is warranted by farmers, nutritionists, veterinarians and researchers alike. Results of supplementation have been rewarding and affordable at pennies on the dollar for dairy farmers in our practice. Prevention of OS could be the secret to making dairy farmers more profitable and cows more comfortable, healthy and productive. ![]()

-
David Krahn
- Veterinarian
- DCountry Hills Animal Health
- Email David Krahn